Why does location matter for health?
In 1948, the World Health Organization defined Health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” This definition has evolved over time to recognize additional factors that have been found to impact health. Driven in part by improved understanding of socioeconomic influences, technological changes, and increased attention on health policy, there has been a growing effort to more thoroughly elucidate factors that determine health. Genetics, individual behavior, social factors, the physical environment, health services and governmental policies all have been found to play a role in health outcomes. Crafting effective policy depends upon a solid understanding of each of these factors, as well as their complex interactions.
Social determinants of health—as distinct from medical care—are increasingly recognized as influencing a broad range of health matters, from access to outcome. According to America’s Health Rankings, when compared with other developed and many developing nations, the U.S. ranks at or near the bottom for health outcomes related to life expectancy. However, data from the Organisation for Economic Co-operation and Development (OECD), which seeks to understand what drives economic, social and environmental change across governments, show that the U.S. continues to exceed other countries in healthcare spending.
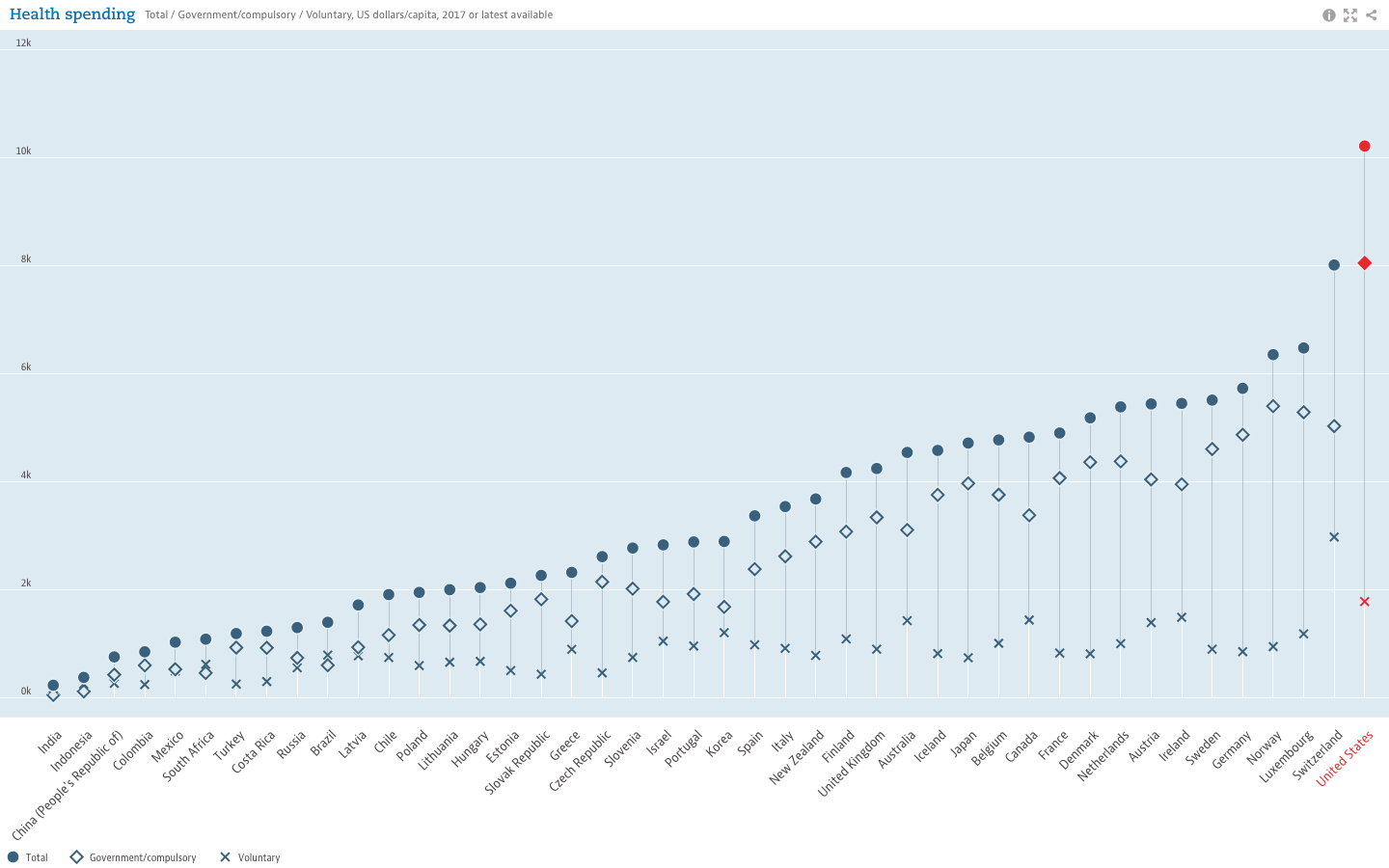
While the United States trails other developed countries in life expectancy (years), it still leads all others in healthcare spending.
Moreover, evidence illustrating the powerful role of social factors in determining health suggests “the effects of medical care may be more limited than commonly thought, particularly in determining who becomes sick or injured in the first place.” Studies have shown that states with a higher ratio of social to health spending had significantly better health outcomes for adult obesity, asthma, mentally unhealthy days, days with activity limitations, and mortality rates for lung cancer, acute myocardial infarction, and type 2 diabetes. Some studies have estimated that medical care is only responsible for 10-15% of preventable mortality in the U.S., indicating that social factors can lead to—or help prevent—poor health outcomes and inequalities.
To address this, the World Health Organization created the Commission on Social Determinants of Health in 2005. By 2008, the Commission concluded in their final report that “inequities are killing people on a grand scale”. Recommendations included improvement of daily living conditions, addressing the inequitable distribution of power, money and resources, measuring and understanding the problem, and assessing impact of action. Growing awareness also led to U.S. Centers for Disease Control (CDC) research, and implementation of a program to advance health equity called Healthy People 2020 which advocates for the creation of “social and physical environments that promote good health for all”, one of their four overreaching goals for the decade.
The Role of GIS
Location affects health. We see dramatic differences in life expectancy between countries, as well as between zip codes. Socioeconomic differences between countries are tied to disparities in health outcomes. Within the U.S., poverty and transportation affects access to healthcare. At a smaller scale, we know that safer neighborhoods, healthy and secure housing, and access to healthy food and open space are associated with healthier populations. U.S. Census data, American Community Survey data, and other sources can help tie such social factors to geography, allowing for better understanding, measurement  and tracking of social determinants of health. Universities, governmental and non-profit organizations now routinely collect such data and utilize GIS to help inform analysis and better decision-making, leading to stronger policies. The Healthy People 2020 Approach to Social Determinants of Health employs a “place-based” organizing framework, organized around Economic Stability, Education, Social and Community Context, Health and Healthcare, and the Neighborhood and Built Environment. Many factors reflecting economic stability, such as poverty and employment, can be mapped within a GIS framework. Mapping education levels, literacy and language, quality of housing, environmental contaminants and areas with high concentrations of chronic disease can help to identify vulnerable populations, reallocate resources and better plan interventions and public education and awareness campaigns. Much of this data is readily available and free of charge. Furthermore, GIS lends itself well to Disparities Analytics, the development of analysis and visualization methods to monitor and report health disparities.
and tracking of social determinants of health. Universities, governmental and non-profit organizations now routinely collect such data and utilize GIS to help inform analysis and better decision-making, leading to stronger policies. The Healthy People 2020 Approach to Social Determinants of Health employs a “place-based” organizing framework, organized around Economic Stability, Education, Social and Community Context, Health and Healthcare, and the Neighborhood and Built Environment. Many factors reflecting economic stability, such as poverty and employment, can be mapped within a GIS framework. Mapping education levels, literacy and language, quality of housing, environmental contaminants and areas with high concentrations of chronic disease can help to identify vulnerable populations, reallocate resources and better plan interventions and public education and awareness campaigns. Much of this data is readily available and free of charge. Furthermore, GIS lends itself well to Disparities Analytics, the development of analysis and visualization methods to monitor and report health disparities.
The Westchester Community Foundation and the Westchester Index
For 40 years, the Westchester Community Foundation, a division of the New York Community Trust, has worked to improve local and regional quality of life in Westchester County, NY by addressing community issues, promoting responsible philanthropy, and connecting donors to critical, local needs. In this capacity, the Foundation, together with the Community Healthcare Association of New York State (CHCANYS) and Westchester County GIS recently developed and released the Westchester Index, a tool developed to help understand social determinants of health in Westchester County. The collaboration relied on data from American Community Survey, the U.S. Census survey, the New York State Department of Health as well as school districts for select health outcomes and socioeconomic indicators. The CDC Social Vulnerability Index (SVI), created by the Geospatial Research, Analysis, and Services Program (GRASP) of the CDC, was also included in the Westchester County Index. The SVI uses 15 U.S. census variables at the census tract level grouped into 4 themes (Socioeconomic Status, Household Composition, Race/Ethnicity/Language, and Housing/Transportation) to help identify communities that may need support in preparing for hazards or recovering from disaster. Westchester County GIS provided detailed data on public transportation, land use
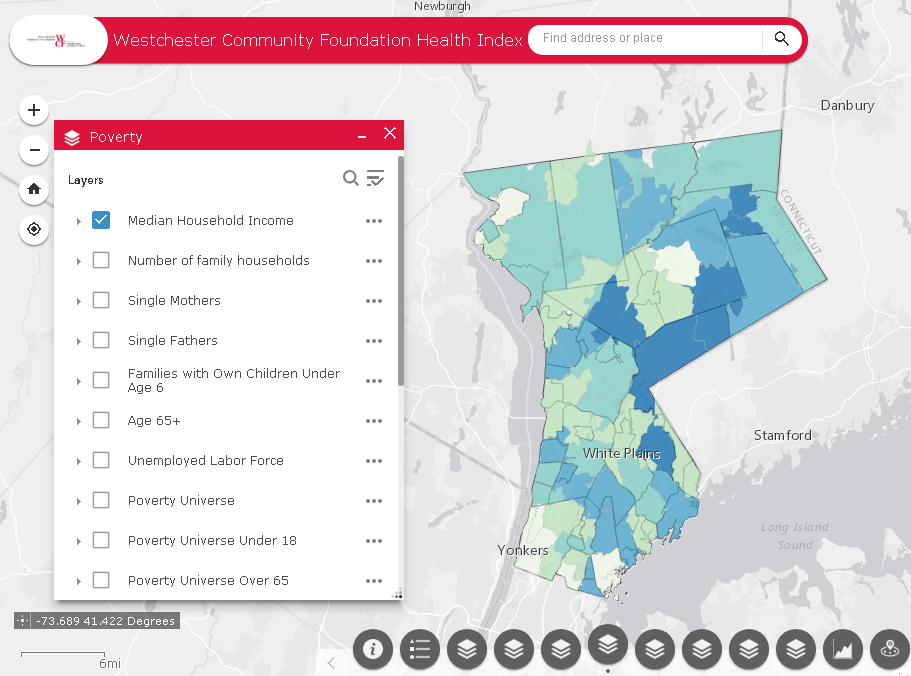
A collaborative effort between Westchester County GIS and the Westchester Community Foundation, the Westchester Index contains data on over 200 indicators reflecting social determinants of health.
categories, as well as locations of environmental hazards. In addition, zip code, census tract and block, school district, municipality, County Legislative district, New York State Senate and Assembly district, and U.S. Congressional district boundaries were provided by Westchester County GIS, allowing for a user to further tailor an analysis. Overall, the Westchester Index contains data on over 200 indicators reflecting social determinants of health. The interactive tool is expected to be used by planning officials, community healthcare networks, school districts, non-profit organizations and others to explore the data and better understand the factors that drive health outcomes in Westchester County, leading to more informed decision-making for greater health equity. View the Westchester Index Story Map here.
Editor’s Note: This article was prepared by Anjali Sauthoff. Ms. Sauthoff is an environmental health scientist currently working with Westchester County GIS to develop integrated approaches that address climate adaptation and community resilience. Her previous research at the Energy Institute at the University of Wisconsin at Madison focused on potential mitigation strategies for reducing transportation-related climate emissions. She received her PhD from Columbia University, where she developed an air pollution exposure model and received training in the health effects of environmental exposures. Her Master’s degree is in Neurobiology from SUNY Stony Brook. She can be reached at ap768@columbia.edu.